Understanding Vitrectomy: A Comprehensive Guide to Retinal Surgery
In the intricate realm of ophthalmic surgery, vitrectomy emerges as a remarkable procedure that holds the power to restore not just sight, but also hope, to individuals grappling with retinal disorders. Imagine a delicate dance within the depths of the eye, where skilled hands wield microsurgical instruments to address a host of conditions that obscure vision and threaten ocular well-being. Vitrectomy, a sophisticated surgical technique, has revolutionised the field of ophthalmology, providing both patients and practitioners with a renewed sense of optimism in the face of retinal challenges.
In this article, we embark on a journey into the realm of vitrectomy surgery, peeling back the layers to uncover the intricacies, benefits, and transformative potential this procedure offers. As we delve into the depths of the eye, we will explore the origins of vitrectomy, the conditions it addresses, the innovative tools and techniques employed, and how lives have been forever changed by this remarkable intervention. From the delicate artistry of the surgeon's touch to the profound impact on the patient's quality of life, vitrectomy surgery emerges as a beacon of light, illuminating the path toward a clearer vision and a brighter future.
What Is Vitrectomy?
Vitrectomy is a surgical procedure performed by ophthalmologists to treat various conditions affecting the vitreous gel and other structures within the eye. The vitreous gel is a clear, jelly-like substance that fills the space between the lens and the retina. It plays a role in maintaining the shape of the eye and assisting with the transmission of light to the retina, which is essential for clear vision.
Vitrectomy involves the removal of a portion or the entirety of the vitreous gel from the eye, often along with other surgical interventions as needed. This procedure is typically conducted using specialised microsurgical instruments and a high-powered microscope for precision.
Here's a detailed overview of the vitrectomy procedure and its applications:
Indications For Vitrectomy
Vitrectomy, a specialised surgical intervention in ophthalmology, is employed to address a spectrum of conditions affecting the vitreous gel and retinal structures within the eye. It serves as a crucial treatment for retinal detachment, macular holes, epiretinal membranes, vitreous haemorrhage, diabetic retinopathy complications, and severe intraocular infections. By skillfully navigating microsurgical techniques, ophthalmologists can remove the vitreous gel and perform necessary procedures to restore retinal integrity, clear obstructions, and ultimately improve vision and ocular health in individuals facing these challenging eye disorders.
Vitrectomy is used to treat a range of eye conditions, including:
Retinal Detachment
Vitrectomy can be employed to repair retinal detachments by reattaching the retina to its original position.
Macular Hole
This procedure can be used to close small macular holes that may affect central vision.
Epiretinal Membrane (ERM)
An ERM is a thin, fibrous layer that can form on the surface of the retina, causing distortion and decreased vision. Vitrectomy can remove the membrane and restore clear vision.
Retinopathy of Prematurity (ROP)
In severe cases of ROP in premature infants, vitrectomy can be used to treat retinal abnormalities and potentially prevent further vision loss.
Vitreous Haemorrhage
In cases of significant bleeding within the vitreous gel, vitrectomy may be used to clear the blood and improve vision.
Diabetic Retinopathy
Vitrectomy can be used to treat complications of diabetic retinopathy, such as vitreous haemorrhage or tractional retinal detachment.
Infections
Severe intraocular infections, such as endophthalmitis, may require a vitrectomy to remove infected vitreous material.
The Procedure
Vitrectomy is a sophisticated ophthalmic surgical procedure that involves the meticulous removal of the vitreous gel, a clear substance within the eye, through small incisions in the sclera. This delicate surgery is performed by skilled ophthalmologists using microsurgical tools and advanced visualisation techniques. During the procedure, the vitreous gel is carefully extracted, and any associated complications, such as scar tissue or haemorrhage, are addressed. Depending on the underlying condition, additional corrective steps, such as retinal reattachment or closure of macular holes, may be taken. The vitreous cavity is then often filled with a sterile solution, gas, or silicone oil to maintain the eye's shape. Vitrectomy holds the potential to restore or enhance vision for individuals afflicted by various retinal disorders, offering them renewed clarity and improved ocular health.
A vitrectomy typically involves the following steps:

Anaesthesia
Vitrectomy is usually performed under local or general anaesthesia, depending on the patient's condition and the surgeon's preference. Anaesthesia administration itself requires careful monitoring and expertise.
Small Incisions
Small incisions are made in the white part of the eye (sclera) to access the vitreous cavity.
Vitreous Removal
Using microsurgical instruments, the surgeon carefully removes the vitreous gel. This step may also involve removing any scar tissue, debris, or blood that may be obstructing vision.
Additional Procedures
Depending on the specific case, the surgeon may perform additional procedures concurrently with the vitrectomy. These procedures could include repairing a retinal detachment, removing scar tissue or membranes, sealing a macular hole, or addressing other complications.
Endolaser or Cryotherapy
In some cases, laser therapy (endolaser) or freezing treatment (cryotherapy) may be applied to the retina to create adhesions, seal retinal tears, or address abnormal blood vessels.
Treatment of Underlying Condition
Depending on the underlying condition being treated, additional procedures may be performed during the vitrectomy. For example, repairing a retinal detachment or sealing a macular hole.
Fluid Replacement
After the necessary procedures are completed, the vitreous cavity may be filled with a sterile saline solution, gas, or silicone oil to maintain the eye's shape and pressure.
Suture or Closure
The incisions are closed with sutures or sealed with other techniques.
Post-Operative Care
Once the surgery is complete, the eye is usually covered with a protective shield or patch, and the patient is monitored in a recovery area. After a period of observation, the patient may be discharged with post-operative instructions for home care.
Recovery And Follow-Up
After the procedure, patients will need to follow post-operative instructions, which may include using prescribed eye drops, continuing to wear an eye shield, and avoiding strenuous activities. The eye gradually heals over time, and patients may experience improved vision as the eye recovers.
Vitrectomy is a highly specialised surgical technique that requires the expertise of a skilled ophthalmologist. The procedure has the potential to restore or significantly improve vision in individuals with various retinal and vitreous conditions, ultimately enhancing their quality of life.
Is Vitrectomy A Major Surgery?
Vitrectomy is generally considered a major surgical procedure within the field of ophthalmology. It involves the removal or manipulation of the vitreous gel, which is a critical component of the eye's structure and function. The surgery requires specialised skills, precision, and advanced microsurgical techniques.
Here are a few reasons why vitrectomy is considered a major surgery:
Surgical Setting
Vitrectomy is typically performed in an operating room using advanced surgical equipment, including high-powered microscopes and specialised tools. The procedure is carried out under sterile conditions to minimise the risk of infection.
Potential Risks
Like any major surgery, vitrectomy carries certain risks and potential complications, such as infection, bleeding, increased intraocular pressure, and retinal tears. These risks underscore the importance of having the procedure performed by a skilled and experienced ophthalmologist.
While vitrectomy is indeed a major surgical procedure, it has proven to be highly effective in treating a variety of serious retinal conditions and complications, often leading to improved vision and overall eye health.

Does Vitrectomy Improve Vision?
Vitrectomy can often improve vision, especially in cases where the surgery is performed to address specific retinal conditions or complications that are affecting visual clarity. The extent of vision improvement after vitrectomy can vary depending on several factors, including the underlying condition being treated, the severity of the condition, the success of the surgical intervention, and the individual patient's overall eye health.
What Not To Do After A Vitrectomy
After undergoing a vitrectomy, it's important to follow your surgeon's post-operative instructions carefully to ensure proper healing and minimise the risk of complications. Here are some general guidelines on what not to do after a vitrectomy:
Avoid Rubbing or Touching the Eye
Refrain from rubbing or touching your operated eye, as this could potentially disrupt the healing process and increase the risk of infection.
Don't Engage in Strenuous Activities
Avoid vigorous physical activities, heavy lifting, or strenuous exercises for the period recommended by your surgeon. Excessive physical strain could put pressure on the eye and affect the healing process.
Do Not Drive Immediately
Your vision may be temporarily blurry or distorted after the procedure due to the effects of surgery and any gas or fluid used during the surgery. It's important not to drive until your vision has sufficiently improved and your surgeon has given you the green light.

Avoid Bending Over
Refrain from bending over at the waist or engaging in activities that could increase intraocular pressure, such as straining during bowel movements. This precaution is especially important if a gas bubble is placed in your eye during the surgery.
Avoid Swimming and Hot Tubs
Stay away from swimming pools, hot tubs, saunas, or other bodies of water until your surgeon gives you the go-ahead. Water exposure can increase the risk of infection.
Don't Skip Medications or Appointments
Follow your surgeon's instructions regarding prescribed eye drops and other medications. Attend all scheduled follow-up appointments to monitor your healing progress.
Avoid Smoking and Alcohol
Smoking and alcohol consumption can negatively impact the healing process. It's advisable to avoid smoking and limit alcohol intake during the recovery period.
Do Not Skip Eye Protection
If your surgeon recommends using an eye shield or protective patch, be sure to use it as directed, especially while sleeping or when you're in environments where accidental contact with the eye could occur.
Don't Use Eye Makeup
Avoid using eye makeup, creams, or lotions around the surgical area until your surgeon gives you clearance. These products could potentially introduce contaminants to the healing eye.
Don't Ignore Signs of Complications
Pay attention to any unusual symptoms such as increased pain, redness, excessive discharge, vision changes, or worsening discomfort. If you experience any of these symptoms, contact your surgeon promptly.
Remember that the specific post-operative instructions may vary based on your individual case and the details of your surgery. Always consult your surgeon or healthcare provider for personalised guidance on what activities to avoid and how to ensure a smooth recovery after your vitrectomy.
How Long Does Vitrectomy Surgery Take?
The duration of a vitrectomy surgery can vary depending on several factors, including the complexity of the procedure, the specific conditions being addressed, the surgeon's experience, and any additional treatments or interventions that may be required. On average, a vitrectomy surgery typically takes anywhere from 1 to 3 hours.
Here are a few factors that can influence the duration of a vitrectomy surgery:
Underlying Condition
The specific retinal condition being treated and the extent of the damage or detachment can affect the time needed to perform the surgery.
Additional Procedures
If the vitrectomy is being performed in conjunction with other surgical procedures, such as retinal reattachment, macular hole closure, or epiretinal membrane removal, the overall surgery time may be longer.
Patient Factors
Certain patient factors, such as the overall health of the eye, the patient's age, and any previous eye surgeries, can impact the complexity of the surgery and the time required.
Surgical Technique
Advances in surgical techniques and technology can also influence the efficiency of the surgery. Surgeons with extensive experience in vitrectomy may be able to complete the procedure more efficiently.
Anaesthesia and Setup
The time required for anaesthesia administration, patient positioning, and setting up the surgical equipment will also contribute to the overall duration.
While the surgery itself may take several hours, the total time spent at the surgical facility will likely be longer due to pre-operative preparations, recovery time after the procedure, and post-operative monitoring.
Your surgeon will provide you with more accurate information about the expected duration of your vitrectomy surgery based on your individual case. As with any surgical procedure, thorough communication with your healthcare provider is essential to fully understand the process and what to expect on the day of surgery.

What Are The Risks Of Vitrectomy Surgery?
Vitrectomy surgery is generally considered safe and effective for treating a variety of retinal conditions. However, like any surgical procedure, there are potential risks and complications that patients should be aware of. It's important to discuss these risks with your ophthalmologist before undergoing vitrectomy. Risks and complications of vitrectomy surgery include:
- Infection - As with any surgery, there is a risk of infection. Intraocular infection (endophthalmitis) is a rare but serious complication that can potentially lead to vision loss if not promptly treated.
- Bleeding - There is a risk of bleeding during or after surgery, which can affect vision and potentially require additional interventions.
- Retinal Detachment - Although vitrectomy is often used to repair retinal detachments, there is a small risk that a detachment could occur or worsen after surgery.
- Cataract Formation - Vitrectomy surgery can increase the risk of developing a cataract (clouding of the eye's natural lens). Most patients will require cataract surgery in the future.
- Increased Eye Pressure - The surgery or gas used during the procedure can temporarily increase intraocular pressure, which may need to be managed post-operatively.
- Macular Edema - Swelling of the macula (macular oedema) can occur after surgery and may temporarily affect vision.
- Vision Changes - While vitrectomy aims to improve vision, there can be temporary changes in vision after surgery, including blurriness, distortion, or changes in colour perception.
- Proliferative Vitreoretinopathy (PVR) - In some cases, scar tissue can develop in the eye after surgery, leading to retinal distortion or detachment.
- Gas or Oil Bubble Issues - If a gas or oil bubble is used to help reattach the retina, there are precautions to follow, such as maintaining proper head positioning to keep the bubble in the desired location.
- Persistent or Recurrent Conditions - In some cases, the underlying condition being treated may not fully resolve, and further treatment or surgeries may be needed.
Many vitrectomy surgeries are successful in improving or restoring vision and addressing retinal conditions. Your ophthalmologist will thoroughly assess your individual case, discuss potential risks, benefits, and alternatives, and provide personalised recommendations based on your specific eye health needs.
What To Expect 3 And 6 Months After Vitrectomy Surgery?
The recovery and healing process after a vitrectomy can vary from person to person and depend on the specific condition being treated. However, here's a general overview of what you might expect 3 and 6 months after vitrectomy surgery:
3 Months After Vitrectomy
- Improved Vision - By this point, you may start to notice improvements in your vision, especially if the surgery was successful in addressing the underlying retinal condition. Your vision may become clearer, and you might experience reduced distortion.
- Follow-Up Appointments - You will likely have had several follow-up appointments with your ophthalmologist to monitor your healing progress. At the 3-month mark, you may have another follow-up appointment to assess your vision and overall eye health.
- Activity Restrictions - Depending on your specific case and the nature of the surgery, some activity restrictions may still be in place. You might still be advised to avoid strenuous activities, heavy lifting, or activities that could increase intraocular pressure.
- Medication - You may still be using prescribed eye drops or medications to manage inflammation, prevent infection, or support healing. Your ophthalmologist will determine the appropriate medication regimen for your recovery.
- Vision Changes - It's possible that your vision may continue to improve over the next few months, but some minor fluctuations or changes in vision could still occur as your eye continues to heal.
6 Months After Vitrectomy
- Steady Improvement - By the 6-month mark, your vision should continue to improve and stabilise further. Any residual visual disturbances or blurriness from the surgery should be minimal.
- Follow-Up Appointment - You might have another follow-up appointment around the 6-month mark to assess your progress. Your ophthalmologist will evaluate your vision, examine the retina, and discuss any remaining concerns or issues.
- Activity and Lifestyle - In many cases, you may be able to gradually resume more normal activities and exercise routines, as long as your ophthalmologist approves. Always follow the guidance provided by your medical team.
- Medication - Depending on your healing progress, your ophthalmologist may adjust your medication regimen or gradually reduce the use of certain eye drops.
- Visual Rehabilitation - If your vision was significantly affected by the underlying retinal condition, your ophthalmologist might discuss options for visual rehabilitation or corrective measures.
Furthermore, these timelines are approximate and can vary based on individual factors. Some people may experience a faster recovery, while others may need more time. Regular communication with your ophthalmologist, adherence to post-operative instructions, and attending scheduled follow-up appointments are essential for a successful recovery after vitrectomy surgery.
How Much Does Vitrectomy Cost In The UK and at My-iClinic?
The cost of a vitrectomy procedure in the UK can vary significantly based on several factors, including the specific region, the hospital or clinic where the procedure is performed, the complexity of the surgery, and whether the patient is receiving treatment through the National Health Service (NHS) or privately.
If you are a resident of the UK and are eligible for NHS treatment, vitrectomy surgery is generally covered by the NHS for medically necessary cases. However, there might be waiting lists and specific criteria that need to be met.
For those opting for private healthcare, the cost of vitrectomy surgery can vary widely depending on the facility, the surgeon's fees, anaesthesia fees, and other associated costs. On average, the cost of a private vitrectomy procedure in the UK could be in the range of several thousand to tens of thousands of pounds.
If you are considering undergoing a vitrectomy or any other medical procedure, it's recommended to consult with a medical professional and the relevant healthcare facilities to get accurate and up-to-date information about the costs involved.
At My-iClinic the cost of vitrectomy starts from £5800 per eye.
What Does The Future Of Vitrectomy Surgery Look Like?
The future of vitrectomy surgery holds exciting possibilities driven by advancements in technology, surgical techniques, and our understanding of ocular conditions. Here are some trends and potential developments that could shape the future of vitrectomy surgery:

Minimally Invasive Techniques
The trend toward minimally invasive surgeries is likely to continue. Surgeons may further refine techniques and instruments, allowing for even smaller incisions, reduced trauma to the eye, and faster recovery times.
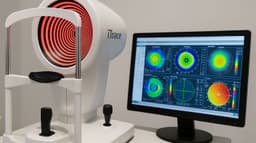
Precision and Imaging
Enhanced imaging technologies, such as high-resolution intraoperative OCT (optical coherence tomography), could provide real-time visualisation of retinal structures during surgery. This would allow surgeons to perform more precise manoeuvres and address conditions with greater accuracy.
Robotic Assistance
Robotic technologies may play a role in vitrectomy surgery, assisting surgeons with delicate manoeuvres and enhancing precision. Robotic systems could offer stability and finer control, potentially leading to improved outcomes.
Gene and Stem Cell Therapies
Advances in gene and stem cell therapies could provide new treatment options for retinal diseases. Vitrectomy procedures might be combined with these therapies to deliver targeted treatments directly to affected retinal cells.
Bioengineered Materials
The development of advanced biomaterials could lead to improved surgical outcomes. Biocompatible materials may be used to replace or support retinal structures, enhancing the success of vitrectomy procedures.

Customised Treatments
Personalised medicine and patient-specific treatments could become more common. Genetic and molecular profiling might guide surgical decisions, optimising treatment plans for each individual.
Artificial Intelligence (AI)
AI algorithms could assist surgeons in planning and executing vitrectomy procedures. AI-driven tools might analyse preoperative images and provide real-time guidance during surgery, optimising outcomes.
Regenerative Medicine
Advances in regenerative medicine could lead to innovative approaches for repairing damaged retinal tissues. Vitrectomy procedures could be combined with regenerative therapies to promote tissue healing and regeneration.
Telemedicine and Remote Monitoring
Telemedicine platforms could enable remote consultations, follow-up appointments, and post-operative monitoring. Patients may have increased access to specialised care and guidance from the comfort of their homes.
Training and Education
Virtual reality (VR) and augmented reality (AR) technologies could revolutionise surgical training and education. Surgeons might practice and refine their skills in realistic virtual environments before performing actual surgeries.
While these possibilities offer glimpses into the potential future of vitrectomy surgery, it's important to note that medical advancements take time to develop, test, and integrate into clinical practice. As technology and medical knowledge continue to evolve, vitrectomy surgery is likely to benefit from these innovations, leading to improved outcomes, enhanced patient experiences, and a brighter outlook for individuals with retinal conditions.
Discover Clarity And Renewed Vision At My-iClinic In London!
Are you seeking advanced and specialised care for retinal conditions? Look no further than My-iClinic, your premier destination for cutting-edge vitrectomy services in the heart of London. Our dedicated team of experienced ophthalmologists is committed to restoring your sight and enhancing your quality of life.
At My-iClinic, we understand the importance of clear vision and personalised care. Whether you're facing retinal detachment, macular hole, or other complex retinal issues, our state-of-the-art facilities and advanced surgical techniques ensure that you're in the best hands. With a track record of excellence and a passion for innovation, our experts tailor each vitrectomy procedure to your unique needs, aiming for optimal outcomes and a brighter, clearer future.
Your journey to improved vision begins with a simple step: reach out to My-iClinic today.
Find out more by Speaking to our team